Why this matters:
- People who are diagnosed with head and neck cancers currently have few treatment options. This cancer significantly affects patients’ quality of life, and its side effects can cause challenges with speech, swallowing and even breathing.
- A growing number of head and neck cancers are found in people who also carry the human papillomavirus, or HPV.
- This research offers great potential to develop new solutions, including immunotherapy, to help activate the body’s immune system so it can eliminate this cancer.
Researchers from Henry Ford Health + Michigan State University Health Sciences have been awarded a $3 million grant from the National Institute of Dental and Craniofacial Research to study new treatments for patients who have head and neck cancer caused by the human papillomavirus, or HPV.
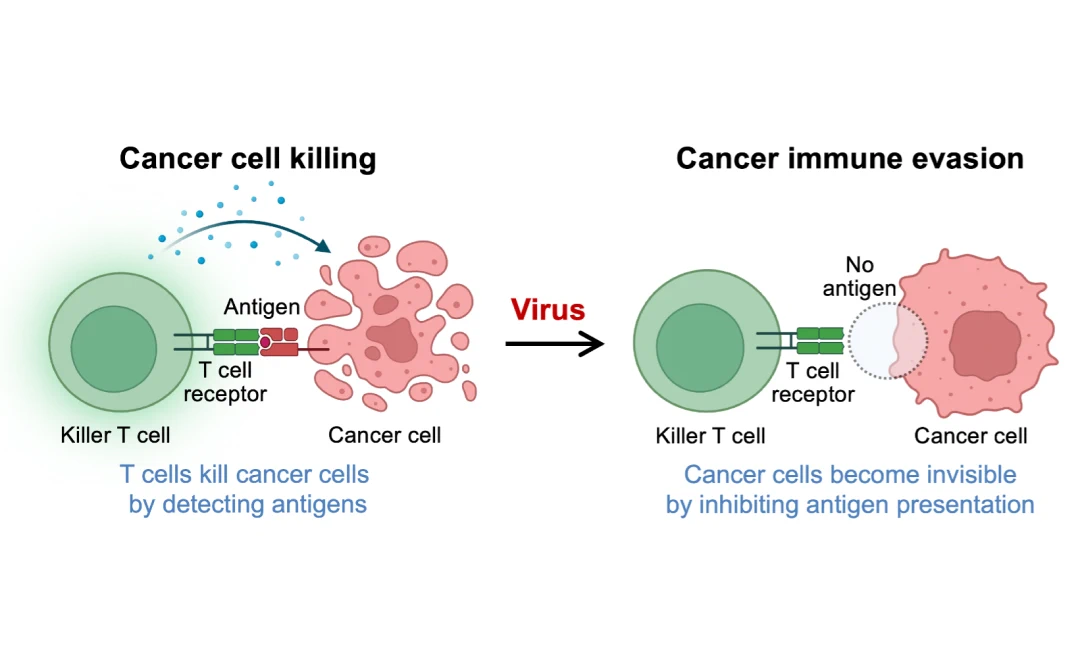
“HPVs cause most cervical cancers and approximately 25% of head and neck cancers, and that number is rising sharply,” said Dohun Pyeon, Ph.D., professor of microbiology, genetics and immunology in the MSU College of Human Medicine and College of Natural Science and principal investigator on this research. “However, scientists don’t know much about how the virus helps these cancers evade the body’s immune defenses. Our research has identified the MARCHF8 protein as a possible culprit, inhibiting the immune system to kill these infected tumor cells. We want to understand how that happens and how to stop it.”
Pyeon says that HPV-positive cancers often bypass the immune system and other natural mechanisms in the body that typically clear early-stage cancer cells very efficiently. And given that an estimated 600 to 700 million people in the world are already infected with HPV, the number of patients who will need treatment for head and neck cancer is expected to rise substantially.
Pyeon and a team of researchers from Henry Ford and MSU discovered preliminary answers about how to improve the body’s detection of these cancer cells with grants from the Henry Ford + MSU Cancer Seed Funding Program and the Strategic Partnership Grant from the MSU Research Foundation.
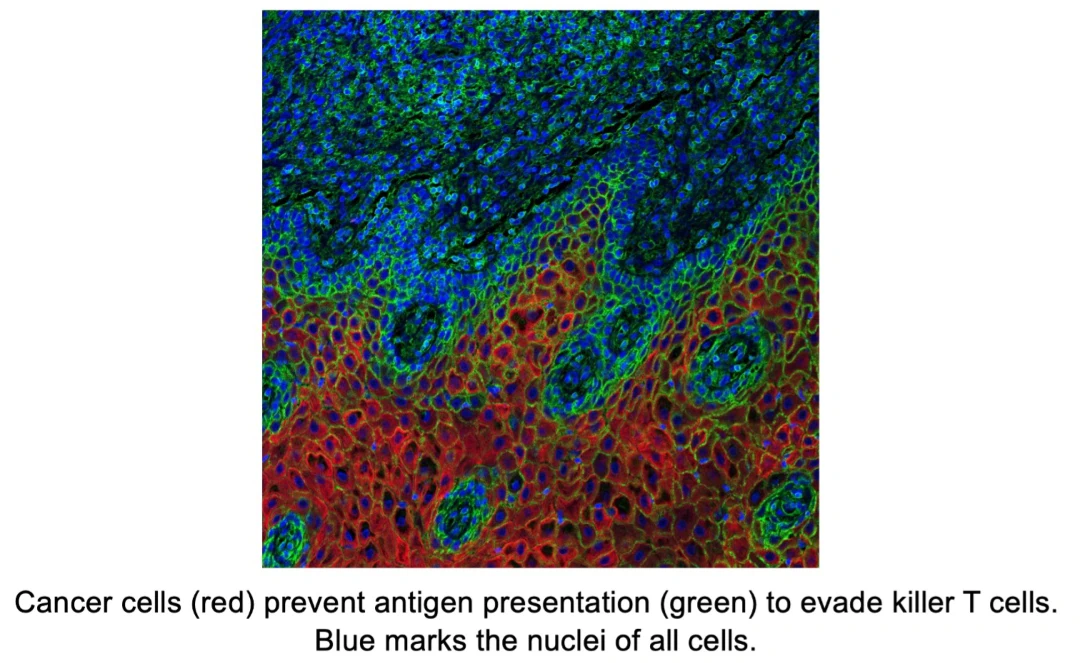
“When cells become infected by a virus, they may develop cancer more rapidly,” said Qing-Sheng Mi, M.D., Ph.D., vice chair for research in the MSU Department of Dermatology, director of the Center for Cutaneous Biology and Immunology, and director of the immunology program of the Henry Ford Cancer Institute at Henry Ford Health. Mi is also professor of medicine at the MSU College of Human Medicine and serves as the co-principal investigator on this project. “These virus-infected cells often downregulate the key molecule enabling the tumor antigen to stimulate the immune system, essentially cloaking themselves from T cell surveillance. Our single-cell analysis of the tumor microenvironment indicates that knockdown MARCHF8 can significantly boost antitumor immunity, making it a potential new therapeutic target.”
“Findings from this research are intended to reduce the intensity of treatment of HPV-positive head and neck cancers and create a better treatment with fewer side effects,” said Steven Chang, M.D., chair of the Department of Otolaryngology/Head and Neck Surgery at Henry Ford Health, interim chair of the Department of Otolaryngology/Head and Neck Surgery at the MSU College of Human Medicine, and a contributor to the research. “We highly recommend the HPV vaccine for those who can get it. Because HPV is a virus, in some patients it can integrate into a patient’s DNA and disrupt the normal cell functions for many years without being eliminated by the immune system. This can lead to cancer, and we want to change that.”