What are the opportunities for nanomedicine in the fight against cardiovascular disease?
I believe that there are tremendous opportunities for nanomedicine to impact cardiovascular diseases. I really think we’re just starting to scratch the surface.
To back that up, last year alone, more articles were published in the field of cancer nanomedicine than have ever been published in the field of cardiovascular nanomedicine. To me, that spells opportunity.
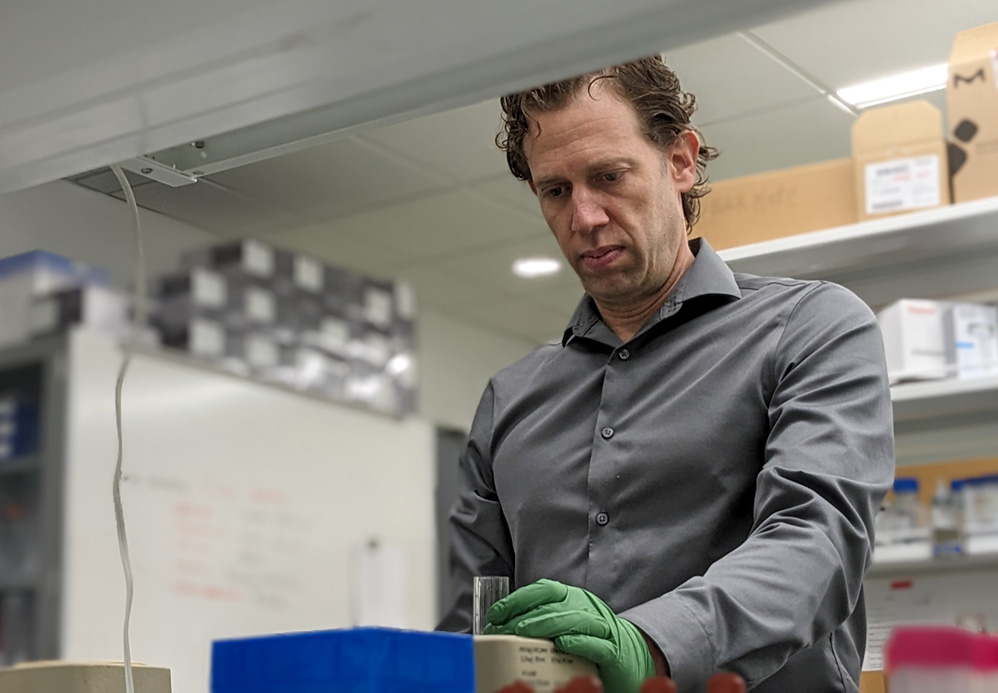
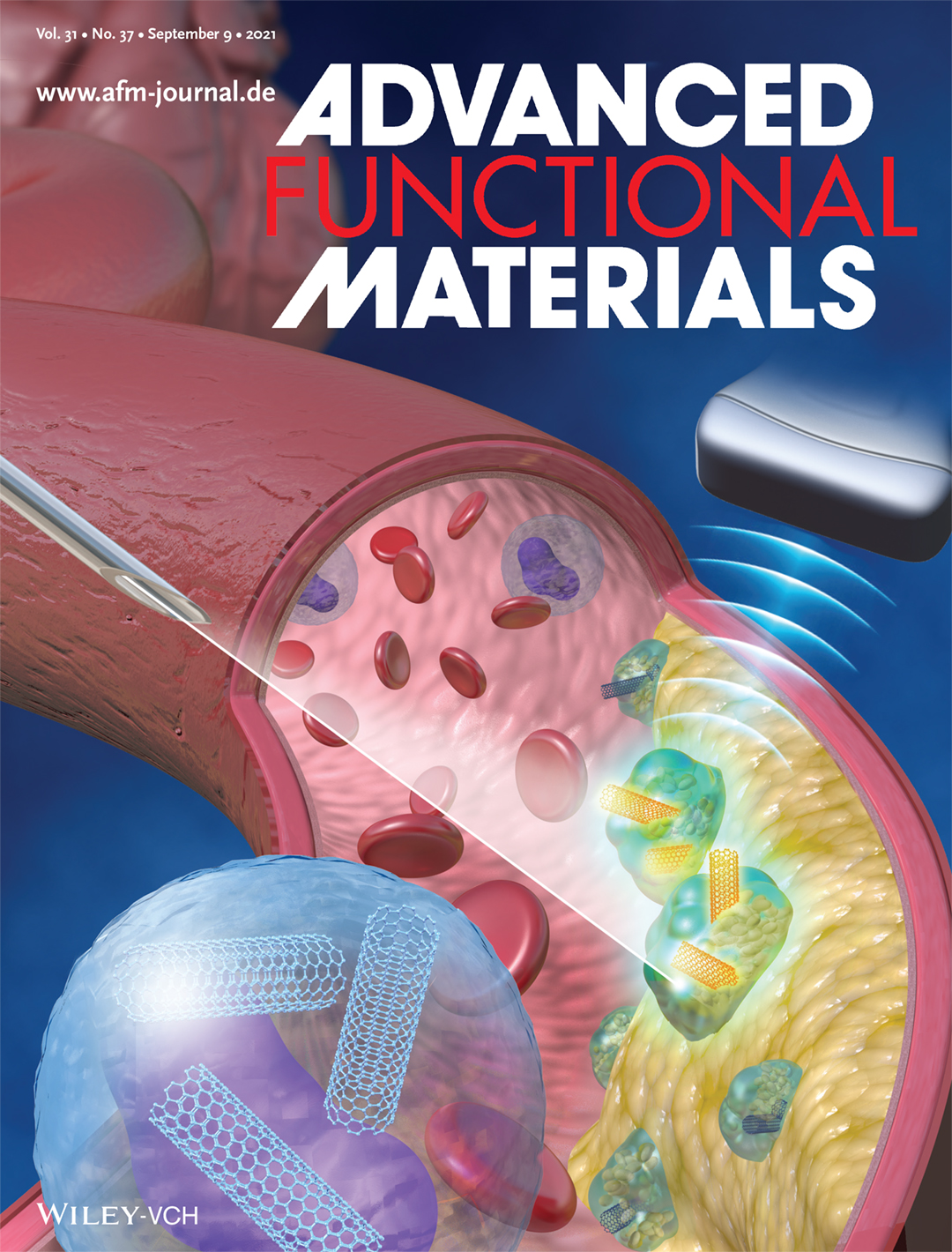
Bryan Smith and his team at Michigan State University also have developed nanomedicines that can image atherosclerotic plaques using a technology that combines light and ultrasound, called “photoacoustic imaging.” This research was featured on the inside cover of the scientific journal Advanced Functional Materials in September 2021. Credit: Advanced Functional Materials
One of the key limitations in current diagnostics and therapeutics is their propensity to cause unintended consequences or adverse side effects. That’s one of the biggest issues in medicine. There are many medications that could be absolutely outstanding for treating a disease, but they’ve been dropped because they have terrible side effects.
In pretty much every medicine ad you see on TV, they’ll show something like people playing with their kids while they talk about all the horrible side effects that medication may cause. By law, they have to tell you what the side effects are and it’s often dozens of different things, sometimes even including consequences like blindness and death. Afterward you’re left thinking, “Would I really want to take that medication?”
What if you could avoid most side effects by getting the medication exactly where you want it to go and nowhere else? That’s what’s so exciting about nanomedicine.
Nanomedicines can be engineered to be extremely, exquisitely selective for particular cells or particular organs, which would then lead to reduced or ideally no side effects. And this is where nanomedicine started. The first nanomedicines didn’t actually treat the disease any better than the regular medicine, but they reduced side effects.
Another area that’s really exciting is nanomedicines can be multifunctional. A nanomaterial can contain a drug, or even lots of drug molecules, but it also can have certain mechanical, immunological and even electrical properties. That’s really attractive, especially in cardiovascular tissues where mechanical, electrical and immunological properties are all critical to proper function.
Can you share an example of what you’re working on in cardiovascular nanomedicine?
Absolutely. One of the things we’re doing is stimulating immune cells essentially to clean up the mess within atherosclerotic plaques.
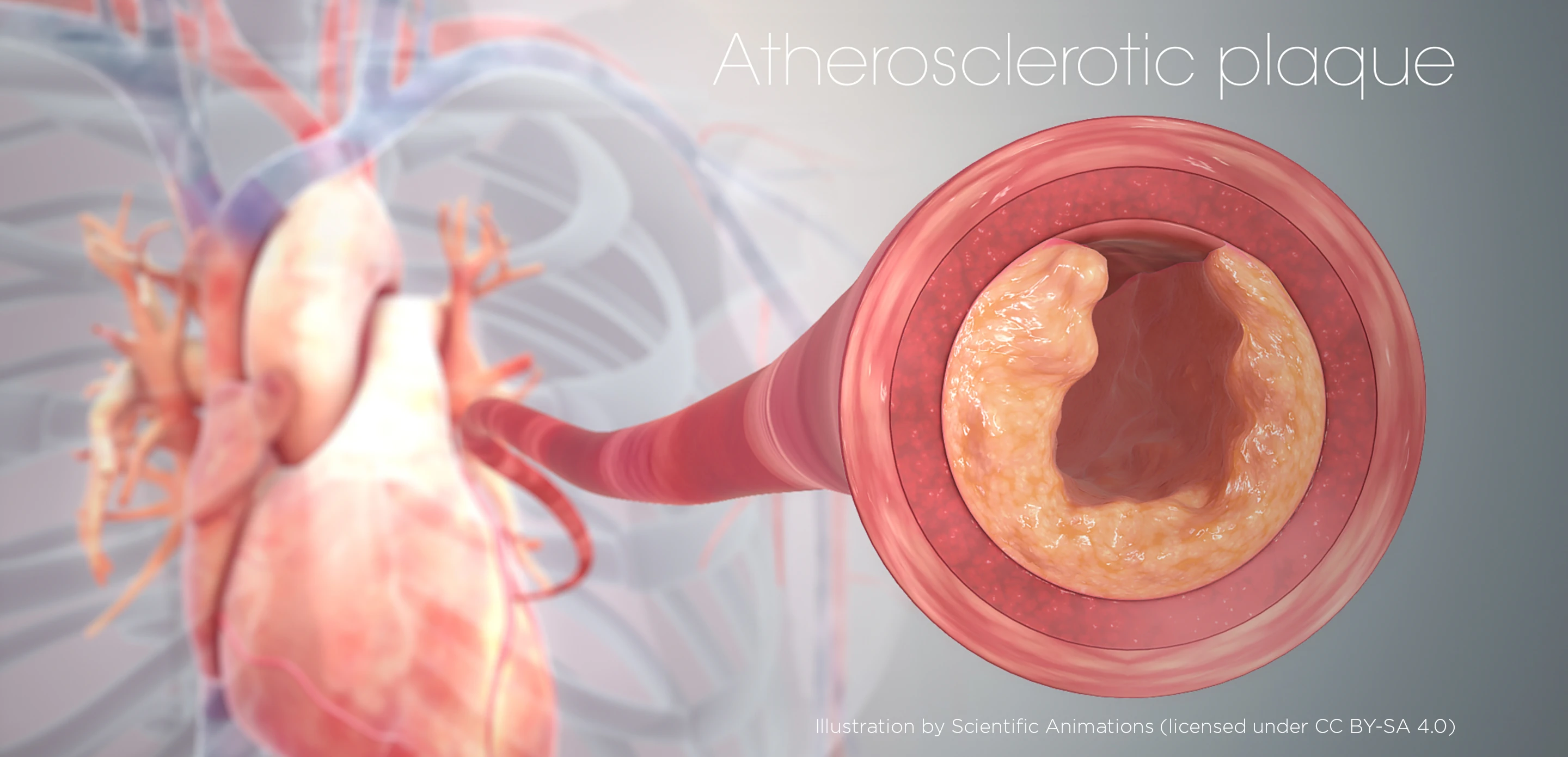
Atherosclerosis is really a critical area of cardiovascular disease. When most people think about cardiovascular disease, they’re thinking about heart attacks. Heart attacks are the primary cause of mortality in cardiovascular disease and atherosclerosis is what causes the vast majority of heart attacks.
That makes atherosclerosis one of the key areas to treat if you want to reverse this statistic of cardiovascular disease being the number one killer of humans worldwide. That’s what we’re doing, and we colloquially refer to it as “taking out the garbage.”
How does that work?
The idea is that cells die throughout your body and typically immune cells called macrophages clean up these dead and dying cells. There’s a constant, healthy process called phagocytosis, in which macrophages eat the dead cells.
That doesn’t happen in an atherosclerotic plaque. There’s a buildup of dead cells, and the macrophages get lazy and don’t do their job. When you need these macrophages the most, they’re not working properly.
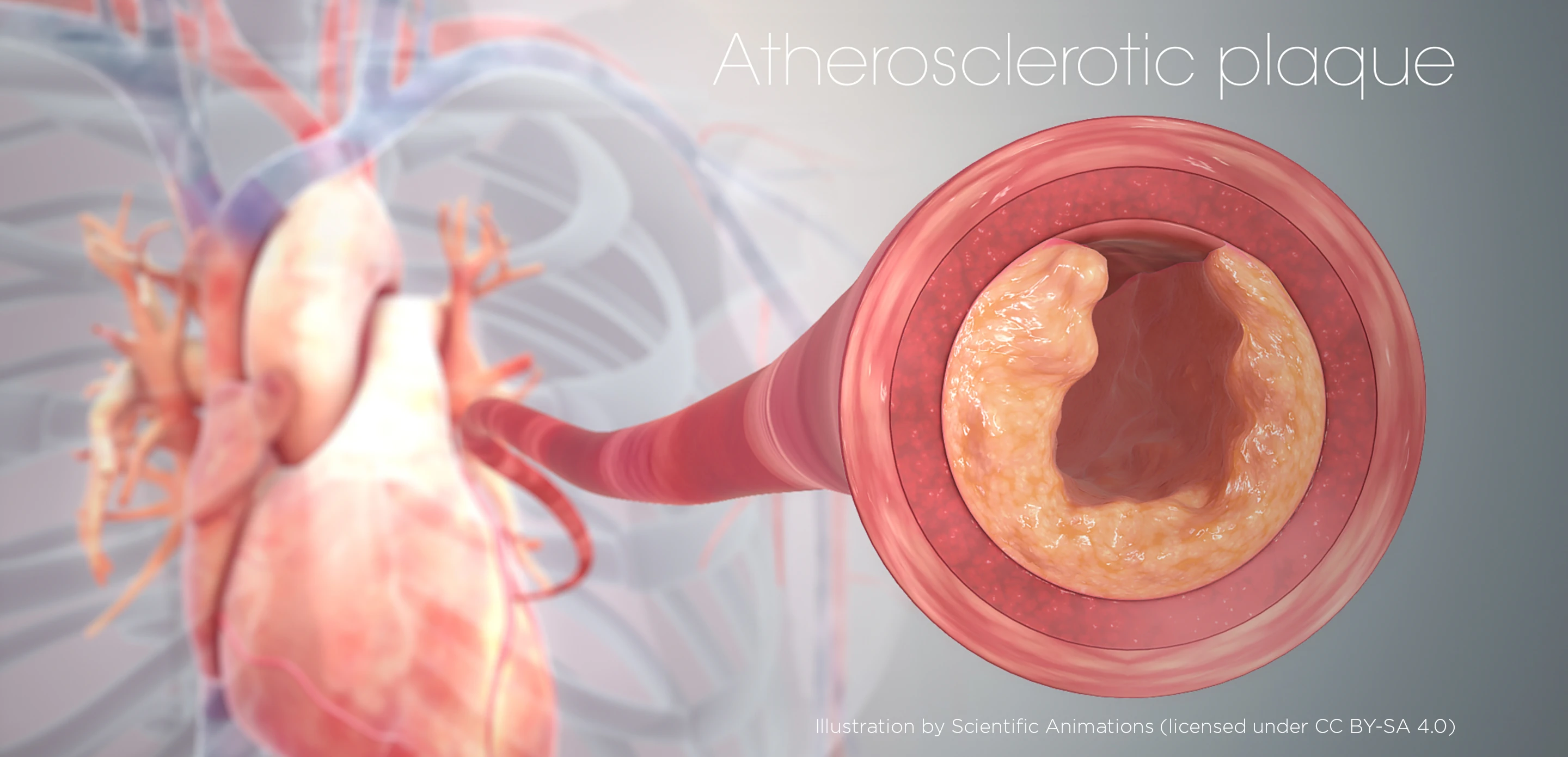
Cells known as macrophages usually help take out the body’s "trash," but they don’t do their job within atherosclerotic plaques, a major cause of heart attacks. At Michigan State University, Bryan Smith and his team are developing nanomedicines to stimulate those cells to resume their trash-collecting role within plaques and better manage vascular disease. Scientific Animations (Licensed under CC BY-SA 4.0)
Instead, there’s a buildup of dead cells that, along with diet and other factors, drives a chronic inflammatory response. The plaque grows bigger and bigger, especially the soft center, making it more and more dangerous because it gets closer to rupturing, which would cause a heart attack.
What we’re developing is a nanomedicine that specifically and selectively targets macrophages and monocytes (the precursors to macrophages), but not other cells. It delivers a drug to those cells that stimulates them to again become good garbage collectors and clean up the plaque.
We’ve shown in preclinical trials that this nanotherapy decreases plaque size, stabilizes plaques and lowers inflammation in the disease site. That’s likely to be critical in the continuing treatment and care of plaques, assuming that, after treatment, patients eat appropriately, exercise and do all the other things necessary to help reverse atherosclerosis.
What that decreased inflammation actually means in the long run is a question we have not yet explored and we hope to examine with animal models and, ultimately, with patients.
Where are nanomedicine therapies for cardiovascular disease in the pipeline now? How long before they might be ready to treat patients?
We’re still early in this field, especially compared with cancer nanomedicine. Looking at U.S. and European clinical trials combined, cancer nanoparticles had around 350 clinical trials, whereas cardiovascular nanoparticles had about 25. The difference is stark.
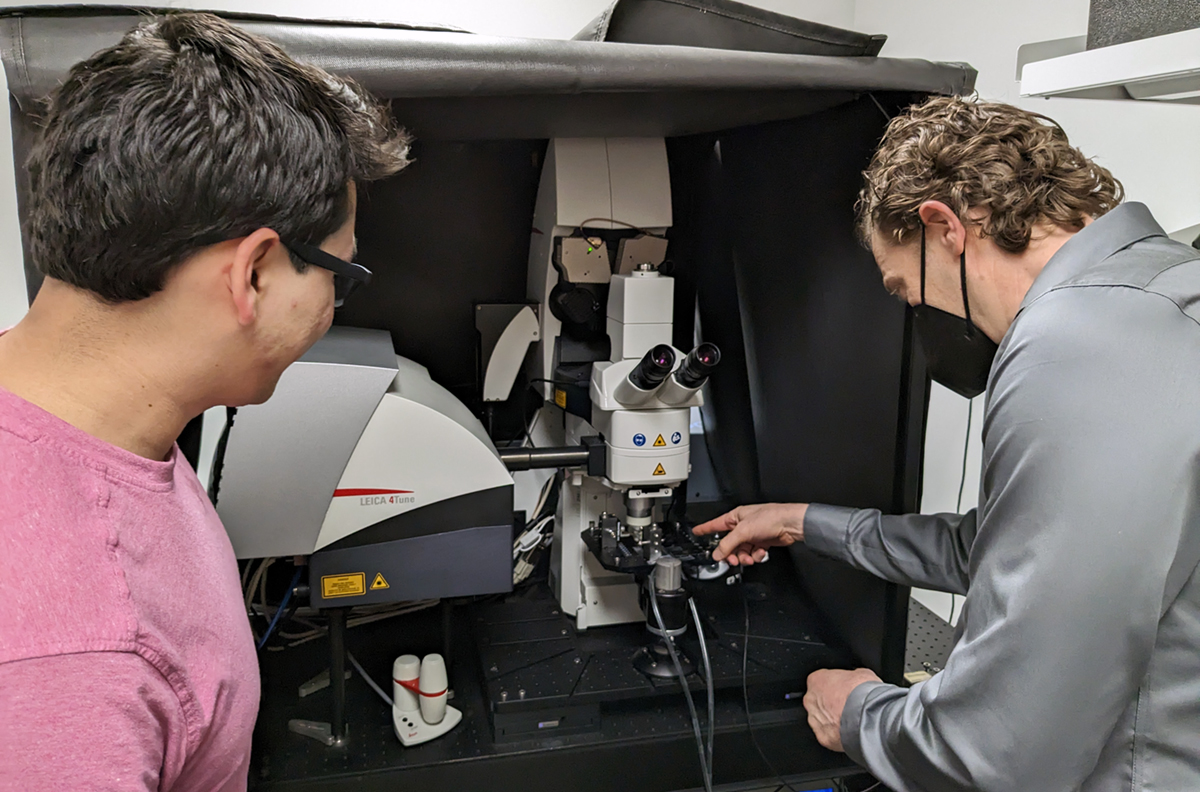
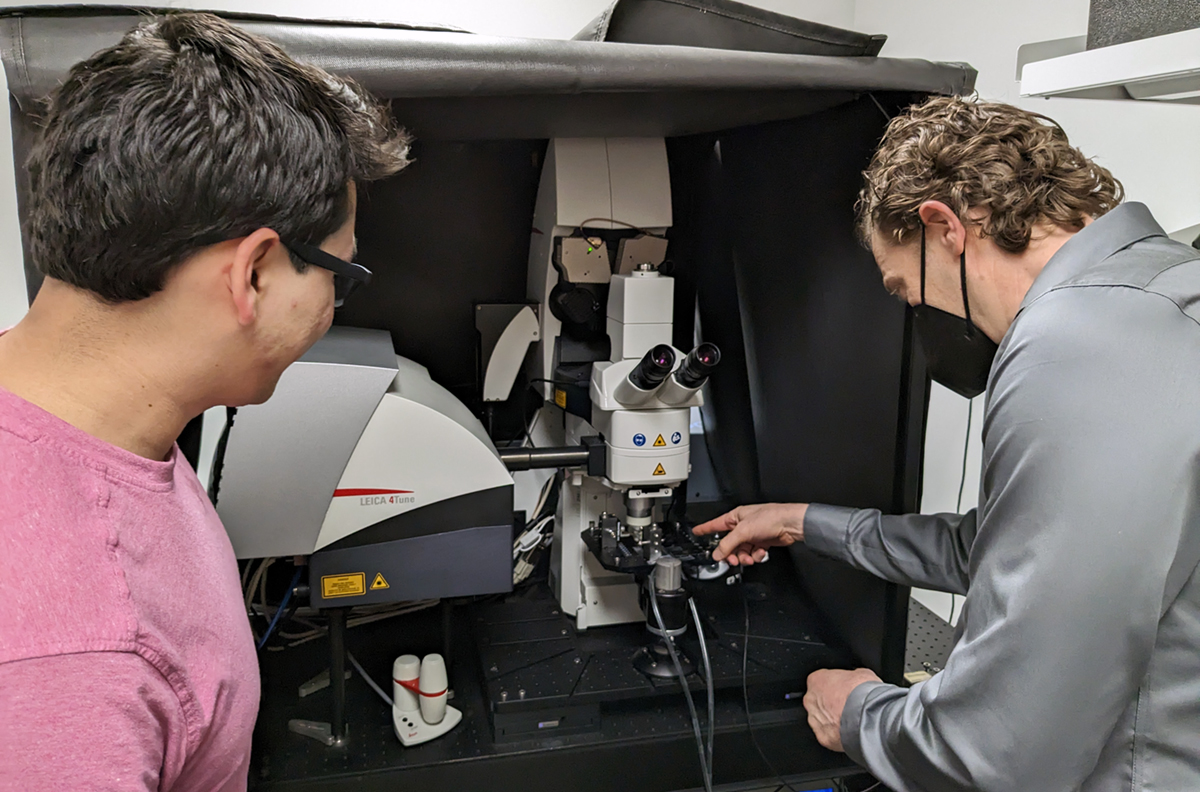
Bryan Smith (right) and Axel Schmitter-Sánchez (left) talk over a microscope in Smith’s lab. Schmitter-Sánchez is a doctoral student on a team led by Assistant Professor Sangbum Park, but groups sharing resources and ideas is a hallmark of research at the Institute for Quantitative Health Science and Engineering at Michigan State University. Credit: Matt Davenport/MSU
But cardiovascular trials do exist, and some are really interesting. There was one using gold-silica nanoparticles with what’s called photothermal therapy in a relatively small patient cohort for atherosclerosis.
With this small cohort, the trial found that these particles did a better job than stents, which is exciting because stents are a major part of cardiovascular health care. Now, that trial has to be repeated on a much larger number of patients to be validated. But that’s just one small example and, as I mentioned, there are 25 nanomaterial-related clinical trials out there right now.
I think we’ll see quite a few more clinical trials within the next five to 10 years, and I hope individuals will be on the lookout for those and consider enrolling if it’s something that they and their physicians agree could help.
Is there anything else you want people to know about nanomedicines and cardiovascular disease?
If this interests someone, they can get involved in local foundation chapters that are dedicated to cardiovascular health. Despite being the world’s number one cause of death, cardiovascular disease doesn’t receive nearly the same level of support that cancer does.
I think heart disease deserves that support and if you believe it, too, support your local chapter of the American Heart Association. Write to your government representatives to make an argument for increasing funding for the National Heart, Lung and Blood Institute.
People also can check out my website and the websites of other researchers doing work in this area and send us questions.