Entertainers like Taylor Swift know the power of an opening act to engage an audience and create a warm welcome for the star performer. When it comes to medical implants, Michigan State University researchers have discovered that using a drug that is a metabolic inhibitor performs like an opening act and makes the body more receptive to medical devices such as pacemakers, replacement joints and dental implants.
“When we surgically place an implant into a human, there will always be an immune response and there’s a chance the implant will be rejected,” said Ashley Makela, senior research associate at the MSU Institute for Quantitative Health Science and Engineering in the College of Engineering. “Our research sought to find novel ways to stop that rejection.”
Makela and a team of multidisciplinary and multi-institutional members used a drug that signals the body to boost or inhibit a particular reaction, called a metabolic modulator. This drug was incorporated into an amorphous polylactide — a biomaterial used to make medical implants — and then the material was implanted in mice.
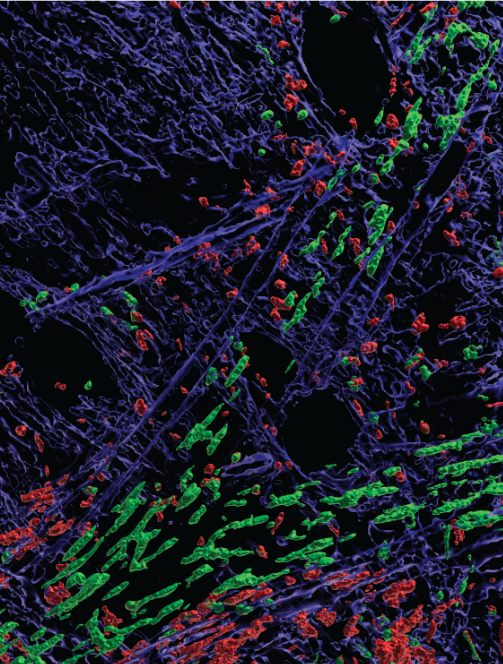
Using intravital microscopy — a technique that allows us to look inside a living subject under a microscope — the researchers imaged different kind of immune cells around the implant site for up to ten weeks.
“Our findings have significant implications for improving patient recovery times, reducing postsurgical complications like chronic inflammation and implant rejection and potentially saving costs,” said Makela. “And they may eventually affect the way medical device manufacturers and pharmaceutical scientists approach medical implants.”
In addition to MSU, the collaborative included team members from the Johns Hopkins University School of Medicine and the University of Michigan Medical School.
“No one person could have done this on their own,” Makela said.
The research was recently published in Nature Biomedical Engineering.