For more than 50 years, the
Leadership in Rural Medicine programs in the
MSU College of Human Medicine have been training future physicians in medically underserved rural communities and small towns across Michigan. The programs encourage and empower students to practice in these areas following graduation. In the Upper Peninsula, this includes the Rural Physician Program based in Marquette, and in Traverse City and Midland, it is known as the Rural Community Health Program.
Students gain experience caring for patients facing health issues prevalent in rural areas, such as higher rates of substance use disorders and chronic conditions. Students also receive training in many settings, from rural hospitals to small outpatient clinics to wilderness survival.
“As someone who was born and raised in rural northern Michigan, the Leadership in Rural Medicine program enabled me to care for the underserved patients that I've always held close to my heart,” says urogynecology fellow Hope Bauer. “The opportunity to be a part of the local community, while learning under the supervision of phenomenal physicians, was incredible.
“Once I complete my fellowship training, I will be joining a practice in western Michigan, where a large portion of the referral base is from rural, underserved locations,” Bauer adds. “The LRM program and my clinical experiences during that time helped me to become the surgeon that I am today.”

Elizabeth Martin, a fourth-year College of Human Medicine student, speaks with physician David Buzanoski during her clerkship in Midland. Martin and other medical students get hands-on experience and become embedded in the health care community through the Leadership in Rural Medicine program. Photo courtesy of the College of Human Medicine
First- and second-year medical students in the MSU College of Osteopathic Medicine have the opportunity to help medically underserved communities while learning clinical skills through its Community Integrated Medicine. Students also provide patients with information on healthy lifestyles, cancer screenings, vaccinations and other local resources tailored to the unique needs of every patient and community.
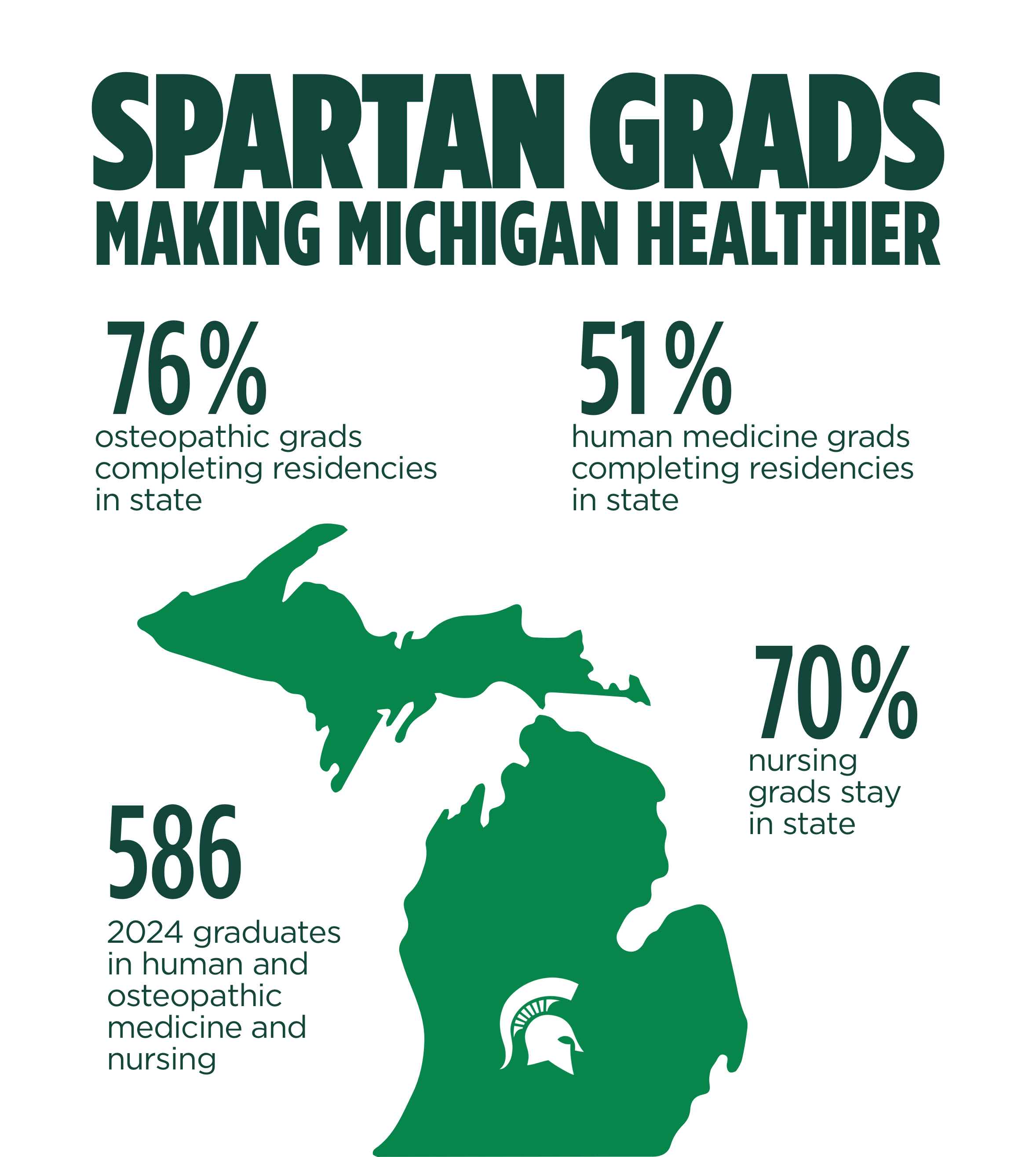
In 2024, 44 of the College of Human Medicine graduates have participated in a Leadership in Rural Medicine program and 380 students were active in the College of Osteopathic Medicine’s program.
Another College of Nursing initiative will greatly increase the number of nurses in the state who care for survivors of sexual assault, with a focus on training in rural communities. The program includes in-person clinical experiences in East Lansing and ongoing remote learning and, by the time the program concludes in December 2024, it will have trained more than 200 nurses from across the state, including many in rural areas and the northern part of the state, as well as the Upper Peninsula.