Researchers from Spectrum Health and Michigan State University College of Human Medicine have determined that COVID-19 patients “cluster” into two main groups: one exhibiting a highly overactive immune system, the other exhibiting a specific type of immune suppression.
The study, published in Frontiers of Immunology, indicates that one group may benefit from immunosuppressive drugs, while the second group may need immune-stimulating therapies. This research demonstrates the uniqueness of individual patients with the same disease.
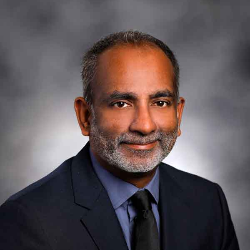
“A greater understanding of severe COVID-19 could help identify which patients are at risk for complications, which would guide more precise therapy,” said senior author Surender Rajasekaran, assistant professor in the MSU College of Human Medicine Department of Pediatrics and Human Development, and research medical director and pediatric intensivist at Helen DeVos Children’s Hospital. “As the virus itself continues to evolve and change, there is immense benefit to understanding the patient’s response to infection.”
Rajasekaran says the research also highlights the importance of precision medicine and personalized care.
“Not only is this beneficial in battling the current COVID-19 health crisis, but it would also be invaluable in treating future infectious diseases,” Rajasekaran said. “Long-term, this data may help clinicians and researchers predict, prevent and treat long-term complications of COVID-19 and any other viral infections.”
Over the course of the pandemic, it has become clear that people have varied responses to infection by SARS-CoV-2. Some become severely ill, requiring complex life support such as mechanical ventilation with prolonged hospitalization, while others have mild infections. It is not yet well understood why some are asymptomatic and others suffer multiorgan failure or death. This unpredictability makes it challenging for clinicians to determine the clinical course and appropriate treatments.
SARS-CoV-2 is an RNA virus that elicits an overactive immune response that damages cells, which in some cases may lead to the chronic illness exhibited by “long-hauler” COVID-19 survivors. Early analysis of this complex immune response could lead to strategies that guide care by selecting the most beneficial therapies and stopping potentially harmful ones.
Rajasekaran said the goal of this study was to evaluate if the patient’s RNA could be used to increase understanding of COVID-19, and whether that knowledge could one day change the approach to the medical treatment of these patients.
The study was conducted on 51 adults hospitalized with COVID-19 at Spectrum Health. The researchers took a close look at each patient’s RNA within the blood. RNA could be used to uncover a body’s response to illness and could guide the clinical team to select the best treatment for any individual. This is the principle of “precision medicine,” an approach where treatments are tailored to one’s unique biological state.
The study team brought together researchers from across the country, representing Spectrum Health, Helen DeVos Children’s Hospital, Michigan State University, Grand Rapids Community College, Ambry Genetics, Calvin University, Grand Valley State University, Davenport University and Children’s Hospital of Pittsburgh.
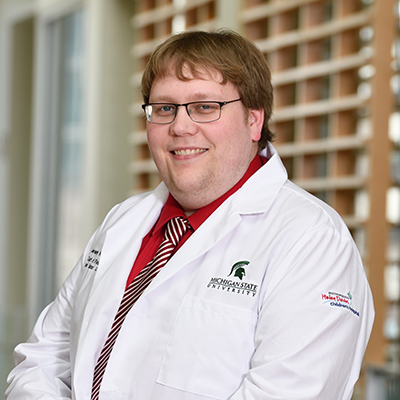
“Just like COVID-19, most infections result in a complex immune response for each patient, with no two individuals having the same biological outcomes,” said Jeremy W. Prokop, the first author of the Frontiers in Immunology paper, and assistant professor at Michigan State University College of Human Medicine. “Through forming strong collaborations between industry, academia, and hospitals we continue to get one step closer to treating each patient based on how the infection changes their body.”
Funding for this research was provided by donors from the Spectrum Health Foundation Gala 2020, the Spectrum Health - Michigan State University Alliance, Michigan State University and the National Institutes of Health.